Understanding and Addressing Chronic Pain After Arthroplasty: A Comprehensive Overview
Total joint arthroplasty, often referred to as joint replacement surgery, has revolutionized the management of debilitating joint conditions, providing relief and restoring function to countless individuals. However, for some, the journey towards pain-free living post-arthroplasty is impeded by the persistence of chronic pain. This blog delves into the phenomenon of chronic pain after arthroplasty, exploring its causes and various strategies to manage and alleviate this challenging aspect of post-surgical recovery.
Chronic Pain After Arthroplasty: A Complex Issue
Chronic pain, typically defined as lasting beyond the expected healing time of three to six months after surgery, can manifest in a variety of ways. It can vary from mild unease to intense distress and debilitating pain, significantly impacting an individual's quality of life and functional abilities. Understanding the causes and mechanisms behind chronic pain post-arthroplasty is vital to tailor effective management strategies. Pain has been defined as a complex, sensory, and emotional experience that is based on actual or potential tissue damage.
Contributing Factors to Chronic Pain
Several factors can contribute to the development and persistence of chronic pain after arthroplasty:
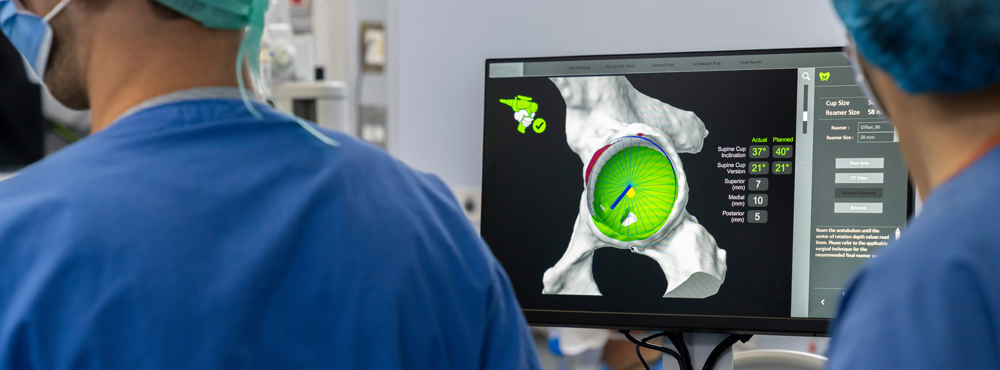
Implant Issues
-
Loosening or malpositioning of the implant can lead to persistent pain and instability in the joint.
-
Implant wear and tear over time may necessitate revision surgery.
Inflammation and Soft Tissue Damage
-
Surgical trauma can cause residual inflammation and damage to soft tissues, triggering chronic pain.
Nerve Injuries
-
Nerve damage during surgery or compression of nerves by the implant can result in persistent neuropathic pain.
Muscle Weakness and Imbalance
-
Inadequate rehabilitation post-surgery can lead to muscle weakness and imbalances, causing ongoing pain and reduced joint stability.
Psychosocial Factors
-
Emotional and psychological aspects, like anxiety, depression, or pain catastrophizing, can exacerbate the perception of pain and hinder recovery.
Strategies for Managing Chronic Pain
Effectively managing chronic pain post-arthroplasty requires a comprehensive, multidisciplinary approach. Tailored strategies can help patients find relief and enhance their overall well-being:
Comprehensive Assessment
Thorough evaluation of medical history, imaging, and physical examinations to identify the specific causes of pain.
Pain Management Techniques
Utilizing a combination of medications, nerve blocks, and physical therapy to manage and alleviate pain.
Physical Therapy and Rehabilitation
Customized rehabilitation programs focusing on strengthening, flexibility, and proprioception to optimize joint function and reduce pain.
Lifestyle Modifications
Encouraging a healthy lifestyle with regular exercise, weight management, and a balanced diet reduces stress on the joints and promotes healing.
Revision Surgery
When necessary, revision surgery may be considered to address implant-related issues and provide pain relief.
Psychotherapy and Counseling
Incorporating psychological support to manage emotional aspects and develop coping strategies for dealing with chronic pain.
Alternative Therapies
Exploring complementary approaches like acupuncture, massage, or yoga to augment traditional pain management techniques.
Conclusion
Chronic pain after arthroplasty is a complex and challenging issue that requires a holistic approach involving medical professionals, physical therapists, and the patients themselves. By understanding the contributing factors and employing a combination of tailored pain management strategies, individuals can work towards alleviating chronic pain and regaining a fulfilling, pain-free life post-arthroplasty.
References:
-
McDowell, M., Park A., & Gerlinger, T. L. (2016). The Painful Total Knee Arthroplasty. The Orthopedic Clinics of North America, 47(2), 317–326.
-
Singh, J. A., & Lewallen, D. G. (2010). Time trends in the characteristics of patients undergoing primary total knee arthroplasty. Arthritis Care & Research, 62(6), 926-934.
-
Beswick, A. D., Wylde, V., Gooberman-Hill, R., & Blom, A. (2012). What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ Open, 2(1), e000435.
-
Wylde, V., Hewlett, S., Learmonth, I. D., & Dieppe, P. (2011). Persistent pain after joint replacement: prevalence, sensory qualities, and postoperative determinants. Pain, 152(3), 566-572.